Menopause and Rheumatoid Arthritis — now there’s two things you don’t want to hear in the same sentence! One is bad enough. I feel a hot flash coming on just thinking about it!
Is there a connection? Does menopause cause Rheumatoid Arthritis? Can menopause make RA worse? Does menopause have any effect at all on RA?Let’s find out!
Menopause and Inflammation
Inflammation is not necessarily a bad thing. If you have an injury such as a cut on your arm, acute inflammation is good, as it helps your body heal faster. However, inflammation that is chronic is a different story. When your body is in a constant state of inflammation that doesn’t go away, well, let’s just say you’re in for a shit storm of epic proportions!
The root cause of most chronic conditions is inflammation. This is particularly concerning for women going through menopause, as inflammation associated with hormonal imbalances may be one of the reasons why women suffer from 75% of all autoimmune disease.
How Do I Calm Down Inflammation?

- Add cooling anti-inflammatory foods to your diet. Choose intensely colored vegetables and fruits, high quality proteins such as grass-fed beef or pastured eggs, and foods rich in omega-3’s like wild caught salmon.
- Avoid processed foods as toxic food can stoke the anti-inflammatory fires. Stick with whole, unprocessed foods instead.
- Move your body. Exercise adds so many benefits to this equation — weight loss + stress reduction = improved joint health.
- Get rid of stress. Burning off stress helps to lower your inflammation markers in your blood. Try meditation, yoga, prayer, therapy — these are just a few options. Stress reduction is never a waste of time — it benefits every area of your life.
- Alternative therapies such as acupuncture, massage, reiki, or chiropractic care can all help alleviate chronic pain and inflammation.
Is Rheumatoid Arthritis Caused by a Hormone Imbalance
Fluctuating levels of estrogen, progesterone, and testosterone may play a part in menopausal inflammation.
Estrogen
Estrogen helps protect joints from inflammation and enhance immunity. As estrogen levels decline, levels of the pro-inflammatory cytokines interleukin-1 and interleukin-6 rise, potentially leading to increased joint pain and stiffness.
Progesterone
What about progesterone? Well, studies have shown that low levels of progesterone correlate with autoimmune disease. An imbalance in the ratio of progesterone / estrogen may contribute to worsening disease symptoms.
If progesterone dips too low, estrogen levels may get too high since there is not enough progesterone available to keep it in check. Estrogen dominance may be the result, leading to immune dysfunction and hormonal imbalances.
Progesterone and cortisol share a common precursor hormone, pregnenolone. When inflammation is high, your body will make extra cortisol to help decrease the inflammation. This equation equals too much cortisol and too little progesterone.
Testosterone
Don’t forget about testosterone! While most studies on low T are done with men, we women have testosterone too! While it may be a pinpoint of the T that a man has, low T in women may have some bearing on RA progression.
A 2013 study found that low testosterone levels in men may mean RA is lurking right around the corner. A recent study found that men with low T have a greater chance of developing Rheumatoid Factor negative RA ( also know as seronegative RA).
Cortisol and Insulin
The hormones, cortisol and insulin, also contribute to this inflammatory stew. Both cortisol and insulin are required for energy metabolism.
When your body is in a constant state of inflammation, it secretes extra cortisol; the excess cortisol, in turn, may lead to insulin resistance, weight gain, low thyroid hormone levels, and impaired immune function.
So, we’ve got estrogen trying to ramp up inflammation and cortisol trying to calm it down. The potential result — autoimmune disease gone wild!
Can Menopause Cause Rheumatoid Arthritis?
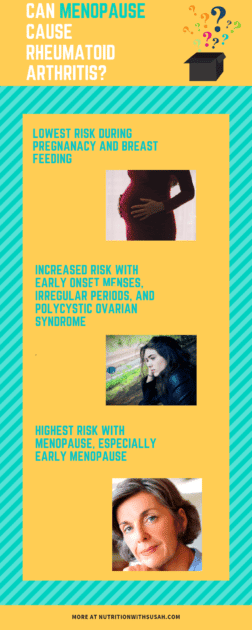
Maybe. The risk of getting RA is lowest during pregnancy, and in women who have breast fed at least 12 months. Often, RA symptoms disappears during pregnancy, which coincides with when estrogen and progesterone levels are at their peak.
Conversely, early onset of menses, irregular periods, and polycystic ovarian syndrome are all associated with an increased risk of RA. But the highest incidence of RA appears to occur in the menopausal years.
Early age at menopause (defined as < 45 years) was associated with the development of rheumatoid arthritis. A cross-sectional study found early age menopause (< 45 years) was associated with RF positive RA. An analysis of the Nurses Health Study found an increased risk of seronegative RA, with the highest risk at early menopause. The results of a Belgium study indicate the average woman in the study had an onset of RA concurrent with the onset of menopause. A 2013 study indicated early menopause was associated with the start of post – menopausal rheumatoid arthritis. However, fluctuating hormones may not be the only menopausal pathway to RA. Menopause increases the production of the interleukin-1, interleukin-6, and tumor necrosis factor alpha. These are the very same pro-inflammatory cytokines that are elevated in those with rheumatoid arthritis and wreak havoc on your joints and organs.
Rheumatoid Arthritis and Hormone Replacement Therapy
Ok, so why not use hormone replacement therapy to treat the symptoms of RA? Oh, if only it were that simple! Unfortunately, the effect of hormone replacement therapy on disease activity is not without controversy. Some studies indicate HRT has little, if any, effect on RA symptoms whereas other studies believe it may be beneficial in RA.
Some research involving a combo HRT of progesterone and estrogen, suggests a decrease in disease activity. However, hormone replacement therapy may increase the intensity of flare-ups, unfortunately.
Let’s not forget those pesky side effects like fluid retention, mood swings, and breast tenderness associated with HRT. High does of estrogen have also been linked to hormone related cancers such as breast cancer. HRT may also increase your risk of heart disease, stroke, and deep vein thrombosis.
CONCLUSION
So what does all this mean? As I’ve long suspected, hormonal fluctuations appear to have an impact on RA, and may even be a root cause of this often devastating illness. While the jury’s still out on whether hormone replacement therapy can help alleviate RA symptoms, menopause seems to play a role in the chronic inflammation of this autoimmune disease.
We’ve all got our own genetic makeup, live in different environments with varying stress levels, all of which impacts our disease risk. I may get RA, but you don’t — there’s no way to know for sure who gets the short end of the stick.
However, there is one thing I do know. Decrease the inflammation in your body and you will decrease your risk of getting an autoimmune disease like rheumatoid arthritis. Make the diet and lifestyle changes you need to make — it may just save you from years of pain and suffering.


